Colon cancer genetic testing
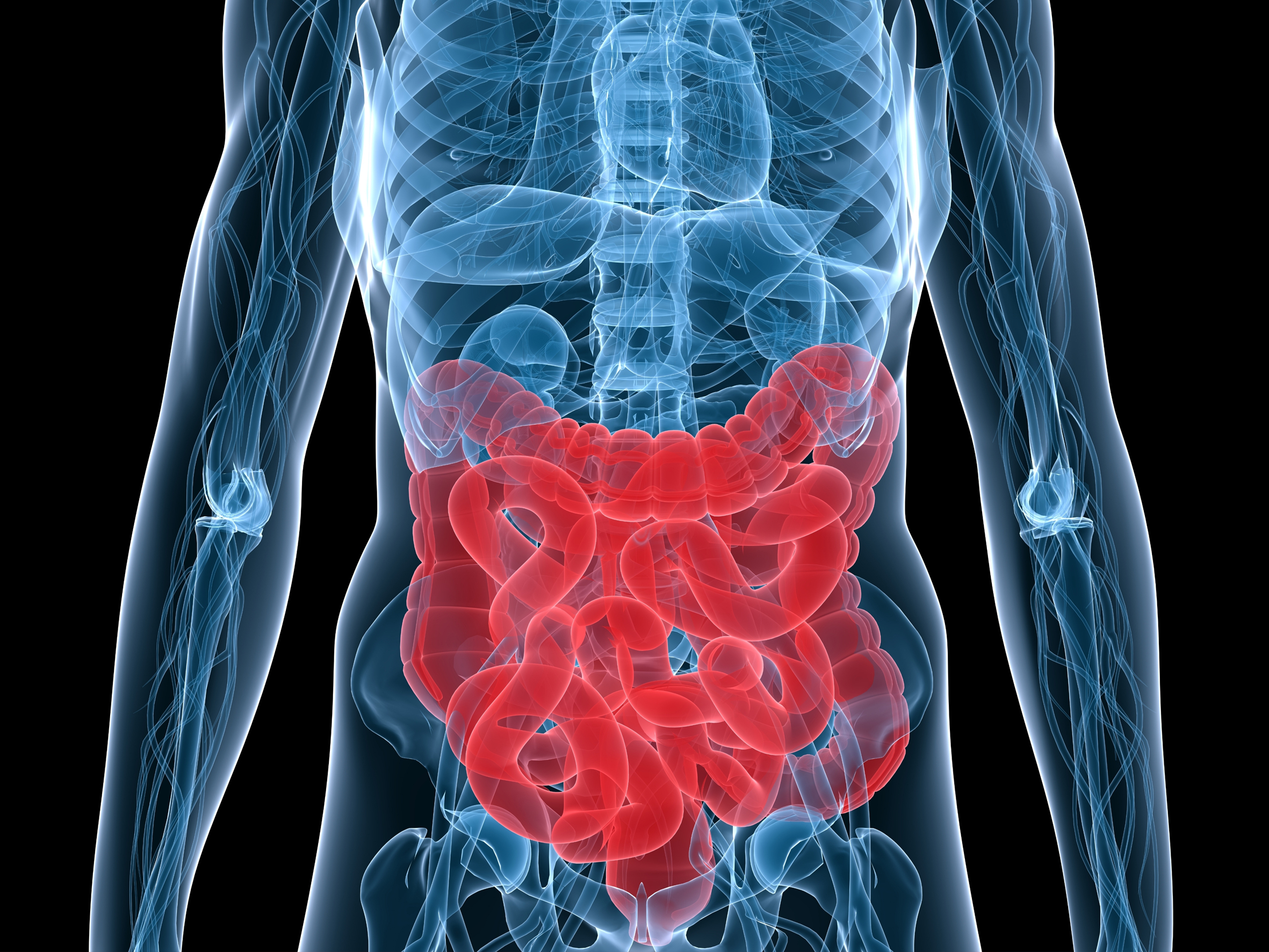
Colon cancer is the Western World’s second most common cause of death due to cancer and 5% of the population suffers from it
How can we help you?
Non-obligation guidance
Fortunately, at IB BIOTECH, we can perform a comprehensive analysis of 100% of the genes that cause this type of cancer in order to rule out hereditary colon cancer or take preventive measures in order to correct a predisposition.
The exact causes of colorectal cancer are unknown in the large majority of cases although we do know that there are some risk factors that favour onset. Some genetic syndromes increase the risk of having colorectal cancer. The most well-known of these are familial adenomatous polyposis (FAP) and hereditary nonpolyposis colorectal cancer (HNPCC) or Lynch syndrome.
What is familial adenomatous polyposis (FAP)?
FAP is a hereditary disease that manifests with multiple polyps (> 100) and it is the cause of 1% of all cases of colorectal cancer. Almost all patients will have colorectal cancer before they reach 50 years of age. Patients frequently also have gastroduodenal polyps and other extradigestive manifestations.
Identifying APC (adenomatous polyposis coli) mutations facilitates diagnosis of the pathology. As well as analysing the APC gene in index cases (people with a FAP diagnosis), it is important that patients are given appropriate genetic guidance so that family members are informed about the associated risks, the importance of monitoring the illness and the significance of the genetic test.
Hereditary nonpolyposis colorectal cancer (HNPCC)
This hereditary disease causes 5% of all cases of colorectal cancer. It is characterised by premature development of colorectal cancer and it often tends to lead to lesions that appear at the same time as, or following, primary colon cancer, in the colon-rectum, as well as tumours in other organs. Mutations in the hMLH1, hMSH2, hMSH6 and PMS2 genes have been identified as responsible for the pathology. Around half of all cases are due to mutations in the hMLH1 gene and almost 50% are due to mutations in the hMSH2 gene. The remainder are due to mutations in other genes (hMSH6, PMS2).
Some of the situations in which having an analysis could prove useful are indicated below.
- Three or more relatives, one of whom is a first-degree level relative compared with the other two, affected by some form of HNPCC neoplasm;
- At least two successive generations affected.
- One of the affected patients was diagnosed before reaching 50 years of age.
The test
The test in order to determine if a person is affected should preferably be done using a blood sample. However, you can also request a kit for collecting oral samples so that it can be done from home.
It is a very simple process. The kit includes sterile cotton swabs that should be used to rub the inside of your mouth. Handle samples with care. Do not touch the cotton swab with your fingers. Once you have taken the sample and it has been appropriately packaged in accordance with the instructions, fill in the forms supplied with the kit and send them to us along with the sample.